
It also showed minimal improvement of overall health-related quality of life after septoplasty. In otolaryngology, the GBI showed improvement in quality of life after different procedures such as intratympanic dexamethasone and intratympanic gentamicin for Meniere’s Disease, rhinoplasty, endoscopic dacryocystorhinostomy (DCR), and tonsillectomy. The questionnaire was designed as an adult otorhinolaryngology (ORL) survey but has been used in other specialties and also in the pediatric age group.
It is a validated, retrospective, single administration test which captures change in health status brought about by a specific event. to measure the change in health status due to an intervention. The GBI was first developed by Robinson at al. However, to date, no comparison has been done on the impact on QOL between primary mastoid obliteration and secondary obliteration. The majority of their patients reported improved QOL and control of the otorrhea afterwards. studied the impact of the secondary mastoid obliteration on QOL using the Glasgow Benefit Inventory (GBI). Very few studies have been published regarding the quality of life (QOL) change due to primary or secondary mastoid obliteration. However, for a problematic non-healing mastoid cavity with chronic otorrhea, a secondary or revision procedure could be done. This has been recommended as a primary procedure at the time of canal wall down mastoidectomy. Palva introduced the use of bone chips and bone pate in combination with a musculo-periosteal flap to obliterate the mastoid cavity. Local fascial musculo-periosteal flaps, autologous grafts such as bone, cartilage and ceramic materials such as hydroxyapatite have been used. Since then various techniques and graft material have been described. In 1911, Mosher introduced the concept of mastoid obliteration. Mastoid obliteration with reconstruction of the bony external ear canal is a procedure that is used to avoid all these complications. The consequences include susceptibility to infection with any water exposure, recurrent otorrhea, the need for frequent cleaning, difficulty with the use of conventional hearing aids and vertigo caused by warm or cold air or water exposure. This is currently the only QOL study comparing these two patient groups.Ī canal wall-down mastoid cavity constitutes a major morbidity to patients with chronic ear disease. Secondary obliterations after revision mastoidectomy scored much higher than primary obliterations. The GBI scores compare favourably with other otorhinolaryngology procedures. This study shows that mastoidectomy with obliteration using autologous cranial bone graft offers a significant QOL benefit. Those with secondary obliteration scored higher, with average scores of 31, general subscale scores of 34, physical health scores of 39, and social health scores of 25. The primary obliteration group had average scores of 19, general subscale scores of 20, physical health scores of 21, and social health scores of 22. Average general subscale scores were 23, physical health scores were 25, and social health scores were 22. Overall GBI scores were improved, with average scores of 22. Twelve were secondary obliteration of an existing canal wall down mastoid cavity. Forty-six were primary obliteration after canal wall down mastoidectomy of a primary cholesteatoma. Resultsįifty-eight patients were interviewed. Patients with cholesteatoma who had mastoidectomy with primary or secondary mastoid obliteration by a tertiary otologist were surveyed using the validated Glasgow Benefit Inventory (GBI), our primary outcome measure. This retrospective observational study was conducted to determine if mastoid obliteration with autologous cranial bone graft following mastoidectomy improves quality of life (QOL). Few have the studied the quality of life benefit that this procedure confers.

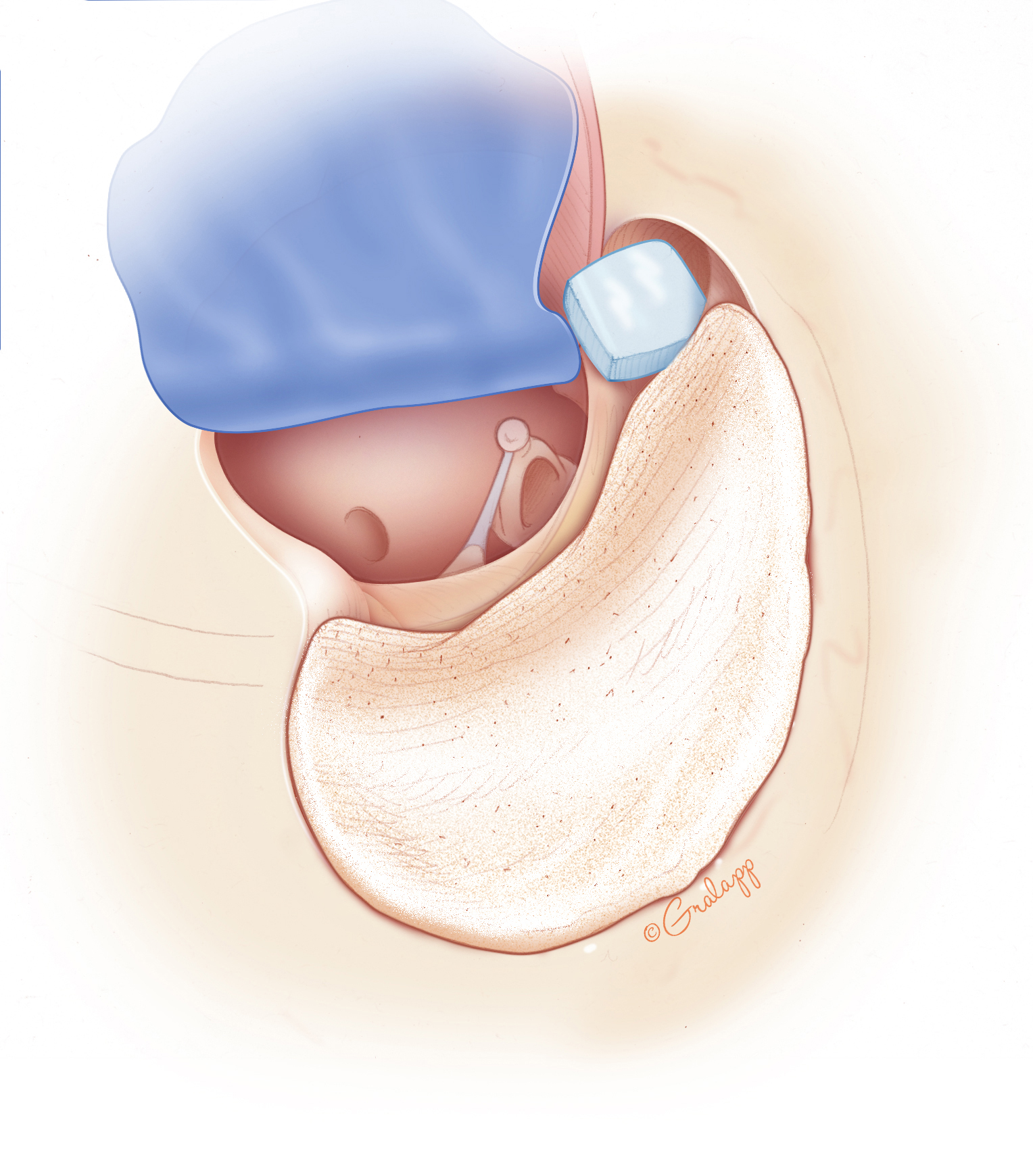
Mastoid obliteration with reconstruction of the bony external ear canal recreates the normal anatomy to avoid such morbidity. A mastoid cavity resulting from a canal wall down mastoidectomy can result in major morbidity for patients due to chronic otorrhea and infection, difficulty with hearing aids and vertigo with temperature changes.


 0 kommentar(er)
0 kommentar(er)
